Expert Corner
How I do a Hexapod Circular Frame
 Hemant Sharma Hemant SharmaHull, United Kingdom |
Introduction
Although circular frames were widely used in Soviet Russia in the 1960s, they only reached the west in 1981. Carlo Mauri, an Italian adventurer, suffered with an infected non-union of his tibia despite multiple surgeries [1]. He subsequently travelled to Kurgan in Russia and underwent surgery by Prof Ilizarov achieving tibial union with resolution of the infection. He in turn introduced the Ilizarov technique to Italian surgeons, who visited Kurgan and invited Prof Ilizarov to Italy to demonstrate the Ilizarov technique.
In the western world, the results reported from Soviet Russia were initially looked at with complete disbelief. However, the circular frame was gradually adopted by a group of surgeons who used it as a last resort for selected cases.
Indications for using a circular frame include leg length discrepancies requiring leg lengthening, non-unions, deformity corrections and bone infections, all of which come under the concept of limb reconstruction surgery. Deformity correction using the circular frame provides the flexibility of ensuring that the limb is perfectly aligned (Figure 1A, 1B, 2A and 2B) to the mechanical axis along with leg lengthening, if required.
In this article, the technique of applying the hexapod circular frame for deformity correction in the tibia is discussed (Figures 4A to 4E). Introduction of the hexapod in the late 1990s, allowed deformity correction simultaneously in all 3 axes which has made deformity correction surgery extremely simple.
Procedure
Understanding the principles of deformity correction is critical [2]. Preoperative planning is essential and can be undertaken either traditionally using a pen-and-paper or using commercial softwares like Trauma Cad. Surgeons must also analyse the secondary effects of deformity correction. Preoperative analysis should cover the following 3 categories:
Local anatomy – previous surgeries, soft tissue status/scarring, current or previous infection. Local soft tissue often dictates the level of the corticotomy.
Patient factors – smoking, co-morbidities, psychosocial status, medication and family support.
Deformity personality – level of deformity, uni/multi-apical deformity, plane of deformity, translation and any leg length discrepancy.
Midshaft deformities are traditionally treated using a 4-ring frame. However, the number of rings and fixation are determined by a multitude of factors such as the type of fractures for trauma, the simplicity or the complexicity or the amount of correction in need.
Any type of anaesthesia can be suitable but the patient should not be paralysed during the surgery. At the preoperative team brief, postoperative pain control should be discussed with the anaesthetist. At our unit, we use ultrasound guided regional blocks and indwelling catheters (which continue postoperatively for 48-72 hours) for pain relief, but an epidural or patient controlled analgesia (PCA) are also suitable.
In our unit and under tourniquet control, a fibular osteotomy is performed, which can be oblique or transverse depending on the direction of the tibial deformity correction and lengthening. At the planned tibial corticotomy site 2, transverse incisions are made, each about 1-2 cm at the edge of the tibia. As a guide, and subperiosteally a vicryl suture is passed but the corticotomy is performed only after the application of the fixator.
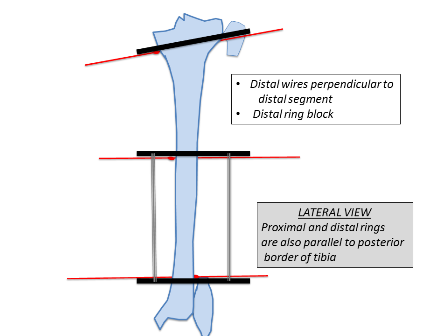
The tibial deformity can be divided into proximal and distal segments. 1-2 rings are aligned perpendicular to each deformity segment (Figures 4B and 4C). A transverse olive wire is then placed as a reference wire. The proximal ring is aligned to the proximal segment in the anteroposterior (AP) and lateral planes, ensuring that the master tab is in the centre of the tibia (Figure 3).
Similarly, the distal ring is aligned to the distal segment in both AP and lateral planes. Struts are then placed connecting both rings. Further one hydroxyapatite coated schanz pins are placed; one in the proximal segment and 2 in the distal segment. In this example 3 wires and one half pin were placed in the proximal segment and 2 wires and 2 half pins were placed in the distal segment. The fibula is usually fixed at both ends with a plain wire or sometimes the proximal tibiofibular joint can be stabilised with a half pin. Fixation can be increased in severe deformities, heavy patients, and where large forces are expected to be counter balanced.
The two/three anterior struts are then removed and a gigli saw (pulling by the vicryl) is passed at the site of proposed corticotomy [2]. Protecting the skin, soft tissue and periosteum, a low energy corticotomy is performed using the gigli saw; cooling with alcohol all the time. Image intensifier is used to confirm that the osteotomy is complete, and only then the anterior struts are placed back to connect the rings. The corticotomy can also be performed using a drill and osteotome technique.
Pin sites are released, and sponges are placed with compression.
Postoperatively foot splint is applied as soon as possible to prevent equinus contracture. First dressing is performed at 48 hours while the nerve catheter is running, ensuring there is minimal pain. First dressing is the most painful to change due to drying and crusting of blood. Patients must be also observed very closely for compartment syndrome.
Full weight bearing is commenced on day 1 and most patients go home in 4 or 5 days. Corrections are usually started on day 10. Lengthening is done at a maximum of 1 mm per day. However, angular corrections can be done much faster depending on patient and local factors such as the compliance of the patients, the age and health.

Outcomes
Despite the initial concerns about once a day corrections and stiffness, the healing index has been similar to the standard Ilizarov frame in elective and trauma surgery [3,4,5,7].
Hexapods are far less complex frames and are ideal for multiplanar corrections. Accuracy of corrections has improved [6] and 3-plane simultaneous correction has simplified the surgeon and patient experience.

Conclusion
Circular frames have gained popularity due to the principles of preserving biology, functional loading and stable fixation achieving excellent results.
Limb reconstruction has evolved significantly in the last 25 years. Patient-centered outcomes have become the primary focus in evolution of limb reconstruction. Therefore, understanding the biomechanics whilst improving the patient’s experience of pain and ability to mobilise postoperatively have become an essential goal to achieve [3,6].
- http://www.mauriziocatagni.it/?page_id=42
- Principles of deformity correction; Dror Paley, Springer Velrag, 2005
- Functional outcomes after tibial shaft fractures treated using the Taylor spatial frame. Henderson D, Barron E, Hadland Y, Sharma H; J Orthop Trauma Volume 29, Number 2, February 2015
- No difference in tibial lengthening index by use of Taylor Spatial Frame or Ilizarov external fixator; Leif Pål Kristiansen, Harald Steen & Olav Reikerås ; Acta Orthopaedica, Oct 2006, 77/5(772-7)
- Correction of Tibial Malunion and Nonunion With Six-Axis Analysis Deformity Correction Using the Taylor Spatial Frame. David S. Feldman, MD, Steven S. Shin, MD, Sanjeev Madan, MD, and Kenneth J. Koval, MDJ Orthop Trauma • Volume 17, Number 8, September 2003
- Fracture healing following high energy tibial trauma: Ilizarov versus Taylor Spatial Frame; Menkaya C, Rigby A, Hadland Y, Barron E, Sharma H; Ann R Coll Surg Engl 2014; 96: 106–110