Update in Orthopaedics
Effect of Spinal Deformity on Pelvic Orientation from Standing to Sitting Position
Chitranjan S. Ranawat, Amar S. Ranawat, Joseph D. Lipman, Peter B. White, Morteza Meftah
DOI: http://dx.doi.org/10.1016/j.arth.2015.11.035
Abstract
Background: The effect of fixed spinal deformities on a functional pelvis from standing to sitting is not fully understood. We aimed to assess the change in preoperative sagittal pelvic tilt angle (SPTA) from standing to sitting in patients undergoing total hip arthroplasty, comparing flexible and fixed spinal deformities.
Methods: Between July 2011 and October 2011, 68 consecutive unilateral total hip arthroplasties were implanted in 68 patients with a mean age of 71 ± 6 years. Fixed spinal deformity was defined as <10° of the change in SPTA from standing to sitting. Preoperative radiographic evaluation included standing (weight-bearing) anteroposterior and lateral pelvic and lumbosacral radiographs and a sitting lateral pelvic radiograph.
Results: The mean standing and sitting SPTA was 3.7° of anterior tilt and 17.7° of posterior tilt, respectively (change of 21.4 ± 12.5°). Seventy-five percent had flexible pelvises, all of which had a posterior tilt from standing to sitting. One patient in the fixed pelvis (1.4%) had a loss of posterior tilt from standing to sitting. The mean change of SPTA from standing to sitting in the fixed and flexible pelvis groups was 5.9 ± 3.5° to 26.7 ± 9.6° of posterior tilt, which was statistically significant (P < .05).
Conclusion: There was a significant change in sagittal pelvic tilt from standing to sitting, especially in patients with a flexible spine, in which the functional anteversion increases with sitting. The patients with a fixed pelvis had significantly less SPTA in standing (less anteversion) with less posterior sagittal tilt in sitting, which should be incorporated in cup positioning.
New York, United States
For total hip arthroplasty (THA), Lewinnek's "safe zone" (40° ± 10° of inclination; 15° ± 10° of anteversion) is often targeted for acetabular component orientation with the goal of minimising the risk of postoperative dislocation [1]. However, two recent papers have questioned whether or not static acetabular component position alone predicts the risk for postoperative instability [2,3]. For any individual patient, it has been shown that sagittal pelvic tilt changes depending on whether the patient is supine, standing or sitting [4]. It follows that the position of the cup is dependent on the 3-dimensional orientation of a patient's pelvis during daily activities, and prior studies have demonstrated how acetabular anteversion and inclination change with alterations in pelvic position [4,5]. Lazennac et al. [6] first described the influence of spinal motion and alignment on pelvic position and acetabular component orientation. However, few studies have examined these relationships in patient cohorts with and without spinal deformities [7,8].
Ranawat et al. [9] explored the effects of fixed versus flexible spinopelvic relationships on the functional position of the acetabular component in a cohort of primary THA patients using frontal and lateral radiographs acquired in standing and sitting positions (Figure 1A-B). Compared to those patients with relatively flexible spinopelvic relationships, they defined those with more rigid spinopelvic motion as having less than 10 degrees of change in sagittal pelvic tilt from standing to sitting position. Of the 68 patients included for the study, over 70% had evidence of spinal pathology and 25% met the authors’ definition of having a stiff spine, or “fixed pelvis”. Flexible patients exhibited slight anterior sagittal pelvic tilt in standing to more substantial posterior tilt in sitting, the effect of which increased functional anteversion of the acetabular component by 0.75 degrees per degree of posterior tilt as they sat. Presumably, increased functional anteversion is protective against posterior dislocation during sitting. For patients with fixed spines, there was significantly less functional acetabular anteversion in the sitting position (i.e. less protection against posterior THA instability). The authors conclude that a dynamic assessment of spinopelvic motion should be part of the preoperative planning for THA. For THA patients with flexible spines, they recommend reproducing native acetabular anteversion, and they speculate that patients with flexible spines do not necessarily require pelvic tilt-adjusted anteversion, as prior publications have suggested [5]. However, they recommend increasing acetabular component anteversion in patients without normal posterior pelvic tilt in sitting.
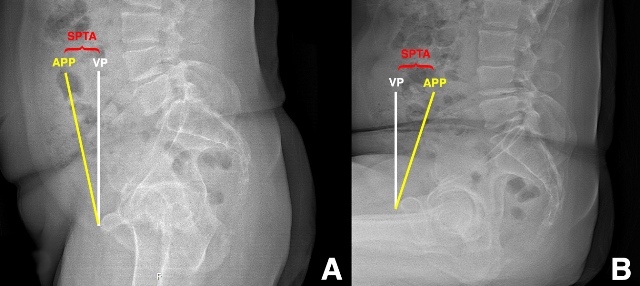
Figure 1: Preoperative sagittal pelvic tilt angle (SPTA) measurements standing (A) and sitting (B) lateral pelvic radiographs. SPTA, sagittal pelvic tilt angle between the anterior pelvic plane (APP, yellow line connecting the antero-superior iliac spines to the pubis) and the vertical plane (VP, white line). There is anterior sagittal pelvic tilt relative to the VP in standing, and there is posterior sagittal pelvic tilt in sitting.
Ranawat et al. [9] elaborate our understanding of the spine-pelvis-hip relationship, and it supports more individualised acetabular orientation targets, considering these dynamic spinopelvic relationships. The next steps are: (1) determining the process to preoperatively plan THA cup positioning, accounting for spinopelvic factors; and (2) identifying techniques/technologies that can reliably execute the plan with a high degree of accuracy. Additionally, longer-term studies are needed to assess changes in functional cup positioning over time. For example, as this study highlighted, there is a high prevalence of concomitant spinal pathology in our hip arthritis patients. As the spine ages, it is reasonable to expect a reduction in spinopelvic motion, and Buckland et al. [10] recently reported that spinal surgery can alter functional acetabular component position in patients with pre-existing THAs.
It should be noted that many THA component orientation analyses ignore half of the range of motion equation: femoral component orientation. Because it is difficult to assess without axial imaging, the femur is often “the forgotten bone”. Yet, optimising femoral component version is critical to maximising range of motion prior to impingement and to minimising bearing surface wear. Furthermore, compared to patients with normal spinopelvic motion, patients with fixed spinopelvic relationships require greater femoral motion relative to the acetabulum to achieve sitting position [8]. Arguably, femoral component position is as important as cup position during functional positions, and the concept of combined anteversion (acetabular anteversion + femoral anteversion) is a biomechanically sound principle to follow in order to avoid impingement and abnormal bearing surface wear [11].
- Lewinnek GE. J Bone Joint Surg Am. 1978;60-A:217–220.
- Esposito CI. J Arthroplasty. 2014;doi:10.1016/j.arth.2014.07.009.
- Abdel MP. Clin Orthop Relat Res. 2016 Feb;474(2):386-91. doi: 10.1007
- Maratt JD. J Arthroplasty. 2014; doi: 10.1016/j.arth.2014.10.014
- Babisch JW. J Bone Joint Surg Am. 2008;doi:10.2106/JBJS.F.00628.
- Lazennec JY. Surg Radiol Anat. 2004;26:136–144.
- Kanawade V. J Bone Joint Surg Am. 2014;96(12):978-986.
- Esposito CI. Clin Orthop Relat Res. 2016 Mar 28. [Epub ahead of print]
- Ranawat CS. J Arthroplasty. 2016; doi: 10.1016/j.arth.2015.11.035
- Buckland AJ. J Bone Joint Surg Am. 2015; doi: 10.2106/JBJS.O.00276.
- Dorr LD. Clin Orthop Relat Res. 2009; doi: 10.1007/s11999-008-0598-4.


















